Introduction: Setting the Scene
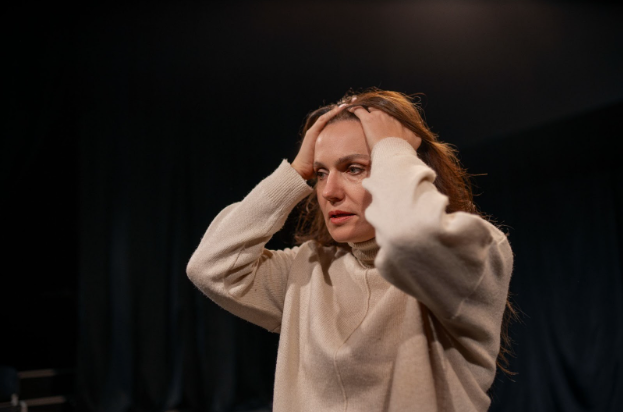
When someone hears a voice calling their name when no one else is around or sees something moving just out of the corner of their eye, the question arises: can bipolar disorder cause hallucinations? Many people associate hallucinations strictly with schizophrenia or psychosis, but the picture is more complex. In certain phases of bipolar disorder, hallucinatory experiences can and do occur.
Hallucinations vs. Psychosis: Clearing Up the Concepts
- Hallucination: A sensory experience in the absence of external stimuli (e.g., hearing voices when no one is speaking or seeing an image that isn’t present).
- Psychotic symptom: A broader category that includes hallucinations, delusions, disorganized thinking, and impaired reality testing.
In bipolar disorder, hallucinations generally arise as a component of a psychotic episode, when mood symptoms are severe enough to distort perception.
When Do Hallucinations Appear in Bipolar Disorder?
Hallucinatory experiences in bipolar disorder are not constant or universal; they tend to cluster around extreme mood episodes. Here’s a breakdown:
Manic or Mixed Episodes
- Hallucinations are more frequently observed when someone is in a full-blown manic or mixed state.
- These psychotic-like symptoms might align with the mood, such as visions of grandeur or voices encouraging high-energy actions. This is known as mood-congruent psychosis.
Severe Depressive Episodes
- Though less common, hallucinations may also emerge during severe depressive phases, often carrying negative or persecutory content (e.g., voices critical of the person).
- These tend to align with the depressed mood—called mood-congruent psychosis—but sometimes may not align, which is known as mood-incongruent psychosis.
Not in Hypomania or Stable Periods
- In hypomanic states (which are milder than mania), psychotic symptoms like hallucinations generally do not occur.
- During euthymic (relatively stable) phases, hallucinations are uncommon unless another underlying cause is present.
Hallucination Types Associated with Bipolar Disorder
- Auditory hallucinations: The most common type. These involve hearing voices or sounds not actually present. They are often mood-congruent—encouraging voices during mania, or critical voices during depression.
- Visual hallucinations: Seeing things like shadows, figures, or flashes of light. These are less common than auditory ones but more likely during manic episodes.
- Tactile hallucinations: Feeling physical sensations (e.g., bugs crawling on the skin). These are rare and typically occur in extreme states.
- Olfactory hallucinations: Smelling things that aren’t there (e.g., burning or rotting odors). These are very rare and more often linked to depressive psychosis.
- Gustatory hallucinations: Unusual tastes, often tied to delusional beliefs like poisoning. These are extremely rare in bipolar disorder.
Hallucinations may be mood-congruent or incongruent, and insight varies from person to person. If these symptoms occur, it’s essential to seek help from a mental health provider. Brain Health USA and a psychiatrist in Los Angeles can provide support, diagnosis, and treatment guidance.
What Mechanisms Might Connect Bipolar Disorder to Hallucinations?
Understanding why hallucinations sometimes occur in bipolar disorder involves examining several interrelated biological and psychological factors:
Neurochemical Imbalances
Bipolar disorder involves fluctuations in brain chemicals such as dopamine and serotonin.
- During manic episodes, excess dopamine activity may lead to increased neural “noise,” making hallucinations more likely.
- In depressive episodes, altered serotonin levels can disrupt sensory processing and lead to perceptual disturbances.
Sleep Disruption and Deprivation
People in manic states often experience severe sleep loss. Sleep deprivation impairs the brain’s ability to filter sensory input and maintain clear boundaries between reality and imagination. This can trigger or worsen hallucinations, especially during prolonged periods without restful sleep.
Stress and Emotional Overload
High stress levels and emotional trauma can increase vulnerability to hallucinations. Intense mood swings combined with overwhelming stress may cause the brain to misinterpret sensory signals or produce false perceptions.
Medication Effects or Interactions
Certain medications used in bipolar disorder may occasionally cause hallucinations as side effects or during withdrawal. Careful management by a psychiatrist in Los Angeles is essential to minimize these risks.
Individual Vulnerabilities and Genetic Factors
Some individuals with bipolar disorder have a predisposition to psychotic symptoms, including hallucinations. Genetic and developmental factors can influence how likely these symptoms are to emerge during mood episodes.
Recognizing Warning Signs: When Hallucinations May Be on the Horizon
A person with bipolar disorder—or their caregivers—can look out for signals that hallucinations might soon appear:
- Rapid escalation of mood symptoms (manic or depressive)
- Severe insomnia or a dramatic reduction in sleep
- Intensifying internal dialogues or intrusive thoughts
- Growing confusion about what is real versus imagined
- Expressing that they hear voices or see things others don’t
- Decline in daily functioning, withdrawal, or difficulty communicating
When these signs emerge, early intervention through mental health support is critical. Brain Health USA can serve as a resource hub, offering guidance, referrals, or advocacy for people navigating such symptoms.
Differential Possibilities: Other Causes to Consider
Because hallucinations are symptoms rather than diagnoses, it is essential to consider competing or contributing causes. Some possibilities include:
- Primary psychotic disorders (e.g., schizophrenia spectrum)
- Substance use disorder or withdrawal
- Neurological conditions (e.g., seizures, brain lesions, neurodegenerative disorders)
- Medical factors (e.g., high fever, metabolic disturbances)
- Medication side effects or interactions
A thorough assessment by a psychiatric professional—such as a psychiatrist in Los Angeles or elsewhere—is necessary to rule in or rule out these alternate explanations. A mental health provider can clarify whether the hallucinations are primarily tied to bipolar disorder or have another origin.
How to Respond When Hallucinations Occur: Practical Strategies & Support
If hallucinations emerge, the path forward often involves multiple complementary responses. Practical strategies include:
- Immediate safety and grounding
- Contacting a mental health provider urgently
- Reviewing and adjusting medication plans
- Engaging in psychosocial support and therapy
- Regulating sleep and reducing stress
- Monitoring and planning for relapse prevention
By responding quickly and comprehensively, a person experiencing hallucinations within bipolar disorder has a better chance of reducing severity, shortening duration, and limiting the impact on functioning.
The Role of Brain Health USA & Local Psychiatric Support in Los Angeles
- Connection and advocacy: Helping individuals locate a qualified psychiatrist in Los Angeles, therapists, or care teams who understand the psychotic features of mood disorders.
- Resource navigation: Offering directories, support groups, peer networks, or educational materials tailored to managing distressing experiences.
- Awareness and stigma reduction: Facilitating conversations that normalize seeking help and reducing shame around hearing voices or seeing things.
- Ongoing follow-up support: Checking in with individuals through telehealth as they progress, helping them stay engaged with care.
Can Bipolar Disorder Cause Hallucinations? Understanding the Connection
- What kinds of hallucinations do people with bipolar disorder experience?
The most common are auditory hallucinations (hearing voices or sounds). Visual, tactile, olfactory (smell), and gustatory (taste) hallucinations can also occur, but are less common. - Are hallucinations in bipolar disorder permanent?
No. Hallucinations usually occur episodically during mood episodes and tend to resolve with proper treatment and mood stabilization. - How are hallucinations treated in bipolar disorder?
Treatment often includes mood stabilizers, antipsychotic medications, therapy, and support from mental health professionals such as psychiatrists and organizations like Brain Health USA. - Can sleep problems in bipolar disorder cause hallucinations?
Yes. Sleep deprivation or disrupted sleep, common during manic episodes, can increase the likelihood of hallucinations. - Is it possible to differentiate hallucinations caused by bipolar disorder from those caused by other conditions?
A thorough evaluation by a psychiatrist is necessary to distinguish bipolar-related hallucinations from those due to other disorders, substances, or medical causes.
Final Thoughts
Hallucinations are a serious but often misunderstood aspect of bipolar disorder. While not everyone with bipolar experiences them, hallucinations can occur during intense mood episodes—especially in manic or depressive phases. Understanding the types, triggers, and mechanisms behind these perceptual disturbances is vital for anyone affected by bipolar disorder and their support network. Recognizing these symptoms early and seeking specialized care can make a significant difference in managing their impact and improving quality of life.
Call to Action
If you or a loved one is experiencing hallucinations or other challenging symptoms related to bipolar disorder, don’t hesitate to reach out for professional help. Organizations like Brain Health USA offer valuable resources and support to connect you with qualified mental health providers. For those in the Los Angeles area, consulting a trusted psychiatrist in Los Angeles can provide personalized care tailored to your needs. Early intervention and ongoing support are key steps toward stability and recovery—take that first step today.
Strict reminder from Brain Health USA to seek a doctor’s advice in addition to using this app and before making any medical decisions.
Read our previous blog post here: https://brainhealthusa.com/what-does-post-traumatic-stress-disorder-feel-like/