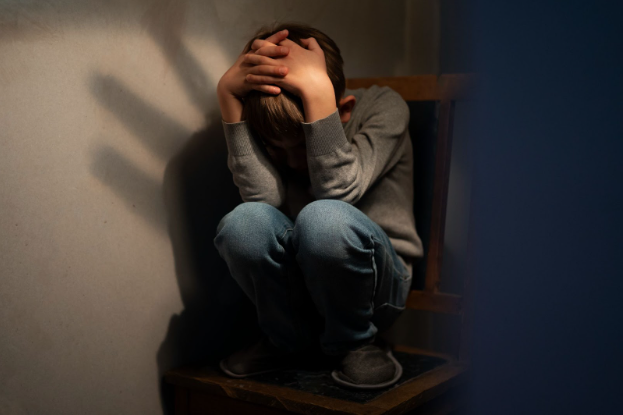
Living with PTSD and depression is often a journey through complex emotional terrain. These two conditions frequently co-occur, intertwining in ways that amplify distress and challenge traditional approaches. At Brain Health USA, a leading mental health clinic, working with an experienced psychiatrist in Los Angeles can provide the specialized care needed to navigate this complexity and support lasting recovery.
How PTSD and Depression Intersect: A Dual Burden
Defining the Conditions
PTSD arises after exposure to one or more traumatic events. Characteristic features include intrusive memories, hypervigilance, avoidance, and emotional numbing.
Depression involves persistent low mood, lack of interest, feelings of worthlessness or guilt, fatigue, and changes in appetite or sleep.
Although these definitions are simplifications, they help clarify how symptoms may overlap.
Why They Co-occur
- Shared biological pathways: Trauma can dysregulate brain circuits and stress hormones, which are also involved in mood regulation.
- Mutual reinforcement: PTSD symptoms—like intrusive thoughts or isolation—can erode mood and lead to depressive episodes. Conversely, depression can lower resilience, making it harder to cope with PTSD triggers.
- Psychological burden: The constant vigilance, guilt, shame, or hopelessness from trauma may tip someone into a deeper depression.
When PTSD and depression exist together, each condition can worsen the other, making recovery more intricate.
Recognizing PTSD with Depression: Key Signals
Because many symptoms overlap, it’s important to stay attuned to both sets of symptoms. If you or someone you care for exhibits several of these signs, seeking help is a wise step.
Symptom Checklist (signs that both may be present)
- Persistent negative thinking — “I’m worthless,” “I’ll never heal”
- Loss of interest in once-pleasurable activities
- Recurrent flashbacks or intrusive memories
- Sleep disruption: nightmares, insomnia
- Emotional numbness or detachment from others
- Heightened irritability or agitation
- Social withdrawal and isolation
- Overwhelming guilt, shame, or guilt about survival
- Difficulty concentrating, indecision
- Low energy or chronic fatigue
When Symptoms Intensify
- You find routine tasks increasingly overwhelming.
- You’re alarmed by sudden surges of fear or dread with no clear trigger.
- You avoid places, people, or memories tied to trauma, even when necessary.
- You notice your mood plummets more frequently and deeply.
- You feel stuck and unable to envision a way out.
If these signs persist for weeks or months and disrupt daily functioning, professional intervention is likely needed.
Key Challenges When PTSD Meets Depression
Understanding the difficulties unique to this dual diagnosis helps in framing more effective treatment and support strategies.
- Fragmented treatment: Traditional approaches often treat PTSD and depression separately. When they coexist, a siloed method may fail to address the interactions between them.
Barriers to Care
- Shame or stigma may discourage seeking help.
- Fear of revisiting traumatic memories may block engagement in therapy.
- Low motivation from depression may undermine consistent participation in treatment.
- Co-occurring conditions like anxiety and substance use disorder add more complexity.
Emotional Overload
The burden of simultaneously managing trauma reminders and a persistently low mood can feel exhausting. It can also distort one’s sense of identity or hope.
A Unique Framework for Recovery (Through the Lens of Brain Health USA)
Brain Health USA can inform a more holistic, person-centered approach to treating PTSD with depression.
Integrative Care Coordination
- Brain Health USA emphasizes collaboration—therapists, psychiatrists, and medical providers working together.
- A psychiatrist in Los Angeles communicates with your therapy team so treatment is harmonized.
Personalized Treatment Plans
Rather than a one-size-fits-all approach, Brain Health USA’s philosophy calls for tailoring therapy modalities (e.g., trauma-focused, behavioral activation) to the individual’s needs. For PTSD with depression, this might mean integrating exposure techniques with strategies to rebuild pleasure and engagement.
Emphasis on Resilience and Support Systems
Rather than focusing solely on symptoms, Brain Health USA encourages fostering strengths, social connection, and coping skills. Cultivating a network of trusted supporters—friends, peer groups, coaches—aligns with this mindset.
Ongoing Monitoring and Adjustment
A psychiatrist in Los Angeles might schedule regular check-ins to adapt medication or strategy when new stressors emerge. Brain Health USA’s model supports tracking changes over time and tweaking care accordingly.
Therapeutic Approaches for PTSD with Depression
Below are key modalities and strategies often woven together:
Psychotherapy Approaches
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): Aims to confront, process, and reframe trauma memories while restructuring depressive thinking.
- Cognitive Processing Therapy (CPT): Helps examine and challenge maladaptive beliefs arising from traumatic events, reducing guilt or shame.
- Behavioral Activation: Encourages reengagement in positive, purposeful activities to counter depressive inertia.
- Eye Movement Desensitization and Reprocessing (EMDR): Supports processing trauma memories with guided bilateral stimulation.
- Mindfulness and Acceptance-Based Therapies: Teach presence and self-compassion to prevent emotional avoidance.
Combining trauma work with mood activation and acceptance strategies is at the heart of treating coexisting PTSD and depression.
Psychiatric Interventions
A psychiatrist in Los Angeles (or in your area) can evaluate whether medication might support symptom relief, especially in severe cases. While medications don’t “erase” psychological wounds, they can provide stability that helps you engage with psychotherapy more effectively.
Adjunctive Strategies
- Peer support groups: Sharing with others who understand can alleviate isolation.
- Lifestyle practices: Regular movement, sleep hygiene, and structure can stabilize mood and reduce reactivity.
- Creative outlets and expressive therapies: Art, journaling, and music can help translate internal pain into external form.
The Role of a Psychiatrist in Los Angeles Within an Integrated Path
A well-informed psychiatrist plays several critical roles when PTSD and depression coexist:
- Diagnostic clarity: Differentiating when trauma, mood, or other factors are primary.
- Medication management: Introducing or adjusting pharmacotherapy to stabilize mood, reduce anxiety, or support sleep.
- Collaborative planning: Working with therapists, care coordinators, and support systems to ensure coherent care.
- Ongoing monitoring: Regularly reassessing progress and side effects through telehealth consultations, enabling timely course corrections as needed.
- Empathy and psychoeducation: Offering explanations, validation, and hope grounded in clinical expertise.
Nurturing Hope When Facing PTSD with Depression
Healing from this dual struggle is rarely linear. But adopting certain perspectives and practices can keep recovery within reach.
- Reframe “relapse” as a curve, not failure: Upswings in symptoms don’t mean failure—just signals to reinforce coping and recalibrate with your care providers.
- Cultivate gentle curiosity: When distress arises, ask, What does this moment want me to notice? Rather than What’s wrong with me? This supports insight over self-blame.
- Sustain connection: Reach out—even in small ways—to trusted friends, support groups, or peer networks. Isolation deepens both PTSD and depression.
- Celebrate micro-victories: Every moment you resist withdrawal, reach out, practice grounding, or sit with pain is progress—even if it doesn’t feel dramatic.
Frequently Asked Concerns
Here are common worries people with PTSD and depression face, along with compassionate guidance:
- What if therapy retraumatizes me? A trauma-informed therapist works at your pace, ensures safety, and supports stabilization before deep memory work.
- Will medication change who I am? In skilled hands like a psychiatrist in Los Angeles, medication is a tool—not identity. It’s there to ease distress so you can engage in healing.
- How long will recovery take? Recovery timelines vary. Some may notice a meaningful change in months; others may take longer. The emphasis is on progress, not strict deadlines.
- What if I can’t stick with treatment? Depression can sap motivation. That’s why integrated models—like the one inspired by Brain Health USA—stress tailored plans, check-ins, and responsive adjustments to maintain engagement.
Final Thoughts: Moving Through the Darkness Toward Whole Healing
Living with PTSD and depression means grappling with memories and moods that stubbornly resist simple solutions. But through integrative, compassionate, and flexible care—guided by approaches championed by Brain Health USA—you can navigate the overlap, reduce suffering, and reclaim connection, purpose, and resilience.
A psychiatrist in Los Angeles who understands trauma and mood interplay can become a key partner in your journey. Together with therapists, peer support, and your own strength, a more sustainable and hopeful path lies ahead.
Whenever you’re ready, stepping toward help is an act of courage—and healing begins in small acts of care, persistence, and belief in possibility.
Strict reminder from Brain Health USA to seek a doctor’s advice in addition to using this app and before making any medical decisions.
Read our previous blog post here: https://brainhealthusa.com/how-common-is-bipolar-disorder/